A mum is raising awareness of a life-threatening infection she almost lost her baby to - if not for the staff at Royal Oldham Hospital.
At 37 weeks into her pregnancy Kathryn Hughes sensed something was wrong, and urged midwives at Wrightington, Wigan and Leigh Teaching Hospitals NHS Foundation Trust (WWL) to induce her - a decision which saved son Joshua Aston’s life.
However, during birth further complications arose and she discovered that her son had sepsis caused by group B Streptococcus (GBS) – a deadly infection which is not typically tested for unless asked.

GBS is a bacterium carried by 20-25 per cent of adults in the UK, typically in the gut or vagina.
Carrying GBS is not an infection or illness, and it rarely causes any symptoms to the carrier and carriage does not need to be treated, as it is classed as normal.
Four years on, Kathryn is warning pregnant women to ask their midwives about GBS.
Recalling Joshua’s birth, the 38-year-old said: “Through my pregnancy I didn’t have any signs or symptoms, I just kept getting told that I had reduced foetal movements – meaning he wasn’t moving as much, so I pushed to be induced at 37 weeks and if I had left it longer he would’ve died.”

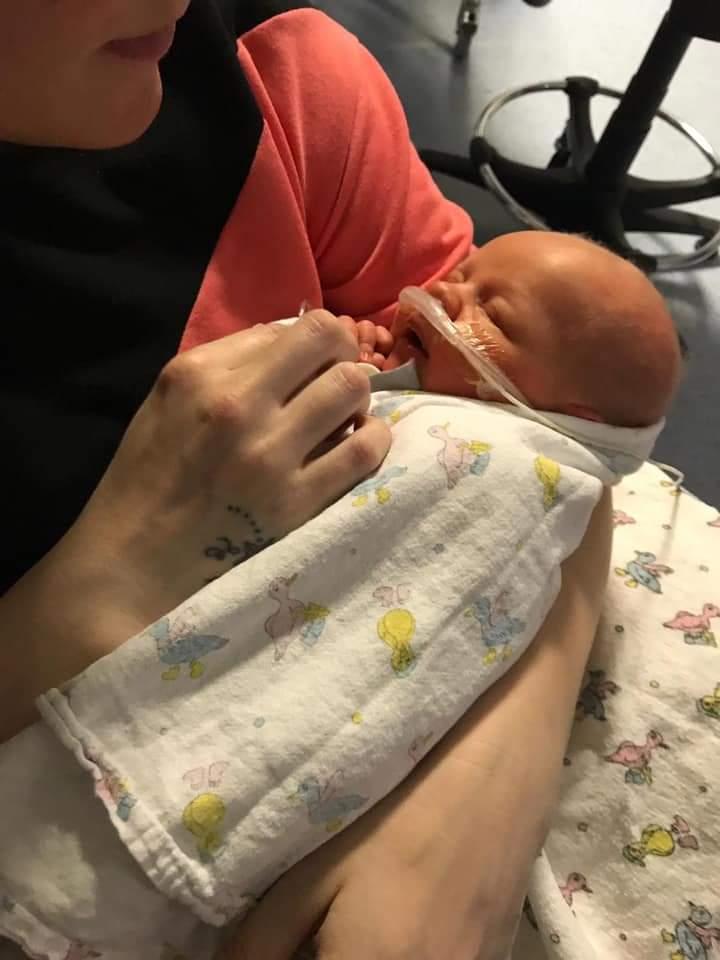
When Joshua was born, he did not open his eyes or take any bottle for two hours before the nurse realised his temperature had dropped at which point he was rushed to the neonatal unit, she explained.
Kathryn continued: “They were putting all these wires on him and he had to have a CPAP (continuous positive airway pressure) machine because he couldn’t breath and his infection levels were high.
“At this point we were still at Wigan hospital and I still didn’t know what was wrong - they just told me that he had an infection and that it was quite common.
“But when he got rushed to Oldham he had to have a lumbar puncture to check for meningitis, and it was only then that I was told he had group B strep.”

On Joshua’s birth Kathryn was told that the next 24 – 48 hours were critical, at which point she began to blame herself for her baby’s poor health.
“I thought it was my fault, I thought with him being so ill it had to be me,” she said.
“It’s just the lack of awareness, it’s not just first-time mums that can come across this – I had two already.
“I didn’t get the opportunity to change my son’s bum for the first time or give him his first feed, which was devastating really because he was in an incubator and he had jaundice too – it was two days before I could touch him.”

Women can pay as little as £37.50 for a GBS test kit online, something the mother-of-three wished she knew about before giving birth to Joshua.
Now, Kathryn, from Wigan, has called for leaflets to be on display on maternity wards for pregnant women to read over before routine check-ups.
She explained: “I still can’t see any leaflets about group B strep – there’s no information out there. If I was told I could pay privately for the testing I would have – £40 is nothing compared to what we had to go through.
“If I had have got tested and it came back positive, while I was in labour they just give you antibiotics – instead Joshua was in hospital with breathing tubes on for 11 days.”
Kathryn continued: “All hospitals should be doing this because that one leaflet could save a baby’s life. People who don’t know me or my story, new mums, won’t ask about getting tested because it’s not a common thing to ask a midwife or a doctor.
“I’m still not convinced that he’s got away with it scot-free, I’m still worried now and I can’t reassure myself that something won’t creep up in the next few years.
“He’s four now and he’s doing well but I can’t get my head around that he’s got away with it and that there’s no lasting damage.”

In response to Kathryn’s story Royal Oldham Hospital is taking part in a large-scale clinical trial which could change how it protects newborn babies from this life-threatening neonatal infection.
Maternity services at Royal Oldham Hospital, part of the Northern Care Alliance NHS Foundation Trust, is participating in the nationwide GBS3 Trial.
GBS3 is a large-scale clinical trial of routinely testing pregnant women for GBS in the UK. It is designed to establish whether testing all pregnant women is better than the UK’s current ‘risk factor’ approach.
It will also compare two different testing approaches - testing at 35 to 37 weeks of pregnancy versus testing in labour.
The trial involves 71 hospitals in England and Wales, including 320,000 pregnant women and people and their babies, and is expected to report its findings in 2025.









Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here